Continuing need program
The continuing need program requires insulin manufacturers to provide insulin to eligible individuals for up to one year, with the option to renew annually. Throughout the year you are determined eligible, the manufacturers will provide your prescribed insulin for a co-pay of no more than $50 for each 90-day supply.
Some individuals with insurance may be referred to a manufacturer’s co-pay program, which waives all or part of the co-pay that the patient normally has to pay, if the co-pay program provides you a better value.
See continuing need FAQ for answers to common questions about the continuing need program.
How to apply
Please see the Patient Information sheet on the Board of Pharmacy website for information and instructions on how to apply. If you need help, contact a MNsure-certified navigator trained to help you through the process.
Who qualifies for the continuing need program?
To be eligible for this program you must:
- Live in Minnesota.
- Present identification proving Minnesota residency in the form of a valid Minnesota identification card, driver’s license or permit, or tribal-issued identification. If you don't have one of these but you have an Individual Taxpayer Identification Number (ITIN), you can provide that instead. If you are a minor under the age of 18, your parent or legal guardian must provide the pharmacy with proof of residency or an ITIN.
- If you are a minor under the age of 18, your parent or legal guardian must provide the pharmacy with proof of residency.
- Have a family income that is equal to or less than 400% of the federal poverty guidelines (FPG) income. See the Minnesota Board of Pharmacy website for more information about the FPG guidelines.
- Not be enrolled in Medical Assistance or MinnesotaCare.
- Not be eligible to receive health care through most federally funded programs. Note: An individual who is enrolled in Medicare Part D is eligible for a manufacturer's insulin safety net program if the individual has spent $1,000 on prescription drugs in the current calendar year and meets the other eligibility requirements.
- Not be eligible to receive prescription drug benefits through the Department of Veterans Affairs.
If you have insurance that covers drugs, you may be eligible to receive insulin on a continuing need basis. However, if you pay $75 or less in out-of-pocket costs for a 30-day supply of insulin, you are not eligible. (Out-of-pocket costs include co-pays, co-insurance and deductibles.)
If you need insulin immediately, see if you qualify for the urgent need program.
Get expert help
You can get help applying for the continuing need program from a MNsure-certified navigator. Navigators are experts at local, trusted community organizations that can help you apply for one of the manufacturer’s programs.
Find a navigator
Use the MNsure Assister Directory below to search for a navigator near you.
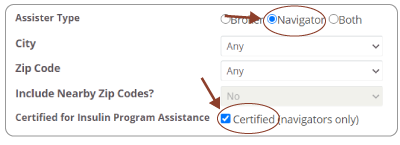 Attention: first change the "Assister Type" to "navigator" and check "Certified for Insulin Program Assistance."
Attention: first change the "Assister Type" to "navigator" and check "Certified for Insulin Program Assistance."
